The
primary organ of respiration in humans are lungs . Their function in the respiratory system is
to extract oxygen from the atmosphere and transfer it into the bloodstream, and
to release carbon dioxide from the bloodstream into the atmosphere, in a
process of gas exchange. In humans, the primary muscle that drives breathing is
the diaphragm. The lungs also provide airflow that makes vocal sounds including
human speech possible.
Functionally,
the respiratory system can be divided into two zones
·
conducting
zone
·
respiratory
zone
Conducting
Zone
The
conducting zone of the respiratory system includes the organs and structures
not directly involved in gas exchange. The gas exchange occurs in the
respiratory zone.The major functions of the conducting zone are to provide a
route for incoming and outgoing air, remove debris and pathogens from the
incoming air, and warm and humidify the incoming air. Several structures within
the conducting zone perform other functions as well. The epithelium of the
nasal passages, for example, is essential to sensing odors, and the bronchial
epithelium that lines the lungs can metabolize some airborne carcinogens.
The
Nose and its Adjacent Structures
The
major entrance and exit for the respiratory system is through the nose. When
discussing the nose, it is helpful to divide it into two major sections: the
external nose, and the nasal cavity or internal nose.

The
external nose consists of the surface and skeletal structures that result in
the outward appearance of the nose and contribute to its numerous functions .
The root is the region of the nose located between the eyebrows. The bridge is
the part of the nose that connects the root to the rest of the nose. The dorsum
nasi is the length of the nose.The apex is the tip of the nose. On either side
of the apex, the nostrils are formed by the alae (singular = ala). An ala is a
cartilaginous structure that forms the lateral side of each naris (plural =
nares), or nostril opening. The philtrum is the concave surface that connects
the apex of the nose to the upper lip.

Underneath
the thin skin of the nose are its skeletal features . While the root and bridge
of the nose consist of bone, the protruding portion of the nose is composed of
cartilage. As a result, when looking at a skull, the nose is missing. The nasal
bone is one of a pair of bones that lies under the root and bridge of the nose.
The nasal bone articulates superiorly with the frontal bone and laterally with
the maxillary bones. Septal cartilage is flexible hyaline cartilage connected
to the nasal bone, forming the dorsum nasi. The alar cartilage consists of the
apex of the nose; it surrounds the naris.The nares open into the nasal cavity,
which is separated into left and right sections by the nasal septum .The nasal
septum is formed anteriorly by a portion of the septal cartilage (the flexible
portion you can touch with your fingers) and posteriorly by the perpendicular
plate of the ethmoid bone (a cranial bone located just posterior to the nasal
bones) and the thin vomer bones (whose name refers to its plough shape). Each
lateral wall of the nasal cavity has three bony projections, called the
superior, middle, and inferior nasal conchae. The inferior conchae are separate
bones, whereas the superior and middle conchae are portions of the ethmoid
bone. Conchae serve to increase the surface area of the nasal cavity and to
disrupt the flow of air as it enters the nose, causing air to bounce along the
epithelium, where it is cleaned and warmed. The conchae and meatuses also
conserve water and prevent dehydration of the nasal epithelium by trapping
water during exhalation. The floor of the nasal cavity is composed of the
palate. The hard palate at the anterior region of the nasal cavity is composed
of bone. The soft palate at the posterior portion of the nasal cavity consists
of muscle tissue. Air exits the nasal cavities via the internal nares and moves
into the pharynx.
Several
bones that help form the walls of the nasal cavity have air-containing spaces
called the paranasal sinuses, which serve to warm and humidify incoming air.
Sinuses are lined with a mucosa. Each paranasal sinus is named for its
associated bone: frontal sinus, maxillary sinus, sphenoidal sinus, and
ethmoidal sinus. The sinuses produce mucus and lighten the weight of the
skull.The nares and anterior portion of the nasal cavities are lined with
mucous membranes, containing sebaceous glands and hair follicles that serve to
prevent the passage of large debris, such as dirt, through the nasal cavity. An
olfactory epithelium used to detect odors is found deeper in the nasal cavity.
Pharynx
In
humans the pharynx is part of the digestive system and also of the conducting
zone of the respiratory system. (The conducting zone also includes the nose,
larynx, trachea, bronchi, and bronchioles, and their function is to filter, warm,
and moisten air and conduct it into the lungs. The pharynx makes up the part of
the throat situated immediately behind the nasal cavity, behind the mouth and
above the esophagus and larynx. The human pharynx is conventionally divided
into three sections: the nasopharynx, the oropharynx and the laryngopharynx. It
is also important in vocalization.In humans there are two sets of pharyngeal
muscles that form the pharynx, determining the shape of its lumen. These are
arranged as an inner layer of longitudinal muscles and an outer circular layer.

The
nasopharynx is flanked by the conchae of the nasal cavity, and it serves only
as an airway. At the top of the nasopharynx are the pharyngeal tonsils. A
pharyngeal tonsil, also called an adenoid, is an aggregate of lymphoid
reticular tissue similar to a lymph node that lies at the superior portion of
the nasopharynx. The function of the pharyngeal tonsil is not well understood,
but it contains a rich supply of lymphocytes and is covered with ciliated
epithelium that traps and destroys invading pathogens that enter during
inhalation. The pharyngeal tonsils are large in children, but interestingly,
tend to regress with age and may even disappear. The uvula is a small bulbous,
teardrop-shaped structure located at the apex of the soft palate. Both the
uvula and soft palate move like a pendulum during swallowing, swinging upward
to close off the nasopharynx to prevent ingested materials from entering the
nasal cavity. In addition, auditory (Eustachian) tubes that connect to each
middle ear cavity open into the nasopharynx. This connection is why colds often
lead to ear infections. The oropharynx is a passageway for both air and food.
The oropharynx is bordered superiorly by the nasopharynx and anteriorly by the
oral cavity. The fauces is the opening at the connection between the oral
cavity and the oropharynx. As the nasopharynx becomes the oropharynx, the
epithelium changes from pseudostratified ciliated columnar epithelium to
stratified squamous epithelium. The oropharynx contains two distinct sets of
tonsils, the palatine and lingual tonsils. A palatine tonsil is one of a pair
of structures located laterally in the oropharynx in the area of the fauces.
The lingual tonsil is located at the base of the tongue. Similar to the
pharyngeal tonsil, the palatine and lingual tonsils are composed of lymphoid
tissue, and trap and destroy pathogens entering the body through the oral or
nasal cavities. The laryngopharynx is inferior to the oropharynx and posterior
to the larynx. It continues the route for ingested material and air until its
inferior end, where the digestive and respiratory systems diverge. The
stratified squamous epithelium of the oropharynx is continuous with the
laryngopharynx. Anteriorly, the laryngopharynx opens into the larynx, whereas
posteriorly, it enters the esophagus.
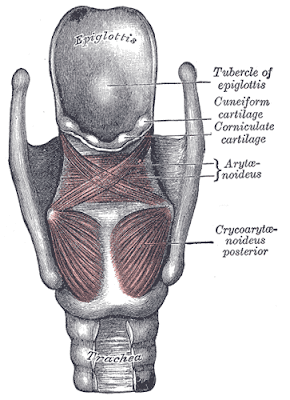
Larynx
The
larynx is a cartilaginous structure inferior to the laryngopharynx that
connects the pharynx to the trachea and helps regulate the volume of air that
enters and leaves the lungs. The structure of the larynx is formed by several
pieces of cartilage. Three large cartilage pieces—the thyroid cartilage
(anterior), epiglottis (superior), and cricoid cartilage (inferior)—form the
major structure of the larynx. The thyroid cartilage is the largest piece of
cartilage that makes up the larynx. The thyroid cartilage consists of the
laryngeal prominence, or “Adam’s apple,” which tends to be more prominent in
males. The thick cricoid cartilage forms a ring, with a wide posterior region
and a thinner anterior region. Three smaller,paired cartilages—the arytenoids,
corniculates, and cuneiforms—attach to the epiglottis and the vocal cords and
muscle that help move the vocal cords to produce speech.
epiglottis
The
epiglottis is a flap made of elastic cartilage tissue covered with a mucous
membrane, attached to the entrance of the larynx. It projects obliquely upwards
behind the tongue and the hyoid bone, pointing dorsally. It stands open during
breathing, allowing air into the larynx. During swallowing, it closes to
prevent aspiration, forcing the swallowed liquids or food to go down the
esophagus instead. It is thus the valve that diverts passage to either the
trachea or the esophagus.The epiglottis gets its name from being above the
glottis (epi- + glottis). There are taste buds on the epiglottis.
Structure
The
epiglottis is shaped somewhat like a leaf of purslane, with the stem attached
to the anterior part of the thyroid cartilage.The epiglottis is one of nine
cartilaginous structures that make up the larynx (voice box). During breathing,
it lies completely within the larynx. During swallowing, it serves as part of
the anterior of the pharynx.
Histology
In a direct section of the
epiglottis it can be seen that the body consists of elastic cartilage. The
epiglottis has two surfaces, a lingual and a laryngeal surface, related to the
oral cavity and the larynx respectively.The entire lingual surface and the
apical portion of the laryngeal surface (since it is vulnerable to abrasion due
to its relation to the digestive tract) are covered by stratified squamous
non-keratinized epithelium. The rest of the laryngeal surface on the other
hand, which is in relation to the respiratory system, has respiratory
epithelium: pseudostratified, ciliated columnar cells and mucus secreting
goblet cells.
Development
The epiglottis arises from the
fourth pharyngeal arch. It can be seen as a distinct structure later than the
other cartilage of the pharynx, visible around the fifth month of development.
Function
The epiglottis is normally
pointed upward during breathing with its underside functioning as part of the
pharynx. During swallowing, elevation of the hyoid bone draws the larynx
upward; as a result, the epiglottis folds down to a more horizontal position,
with its superior side functioning as part of the pharynx. In this manner, the
epiglottis prevents food from going into the trachea and instead directs it to
the esophagus, which is at the back. Should food or liquid enter the windpipe
due to the epiglottis failing to close properly, the gag reflex is induced to
protect the respiratory system.
Gag reflex
The glossopharyngeal nerve (CN
IX) sends fibers to the upper epiglottis that contribute to the afferent limb
of the gag reflex. (The gag reflex is variable in people from a limited to a
hypersensitive response.) The superior laryngeal branch of the vagus nerve (CN
X) sends fibers to the lower epiglottis that contribute to the efferent limb of
the cough reflex.This initiates an attempt to try to dislodge the food or
liquid from the windpipe.
The trachea, colloquially
called the windpipe, is a cartilaginous tube that connects the pharynx and
larynx to the lungs, allowing the passage of air, and so is present in almost
all air-breathing animals with lungs. Only in the lungfish, where the lung is
connected to the pharynx and the larynx, is it absent.The
trachea extends from the larynx and branches into the two primary bronchi. At
the top of the trachea the cricoid cartilage attaches it to the larynx. This is
the only complete ring, the others being incomplete rings of reinforcing
cartilage. The trachealis muscle joins the ends of the rings and these are
joined vertically by bands of fibrous connective tissue – the annular ligaments
of trachea. The epiglottis closes the opening to the larynx during swallowing.
trachea
The trachea develops in the
second month of development. It is lined with an epithelium that has goblet
cells which produce protective mucins. An inflammatory condition, also
involving the larynx and bronchi, called croup can result in a barking cough. A
tracheotomy is often performed for ventilation in surgical operations where
needed. Intubation is also carried out for the same reason by the inserting of
a tube into the trachea. From 2008, operations have transplanted a windpipe
grown by stem cells, and synthetic windpipes; their success is however doubtful.

The human trachea has
an inner diameter of about 25 millimetres (1 in) and a length of about 10 to 16
centimetres (4 to 6 in). It commences at the lower border of the larynx, level
with the sixth cervical vertebra.
Inside the trachea at the level of the fifth thoracic vertebra (T5) there is a
cartilaginous ridge known as the carina of trachea which runs across from the
front to the back of the trachea and marks the point of bifurcation into the
right and left primary bronchi. The carina is opposite the sternal angle and
can be positioned up to two vertebrae lower or higher, depending on breathing.A
ring of hyaline cartilage called the cricoid cartilage forms the inferior wall
of the larynx and is attached to the top of the trachea. The cricoid cartilage
is the only complete ring of cartilage in the trachea. Below this there are
from fifteen to twenty incomplete C-shaped tracheal rings or tracheal
cartilages, also of hyaline, that reinforce the front and sides of the trachea
to protect and maintain the airway. This leaves a membranous wall at the back,
(about a third of the ring's diameter) without cartilage. The cartilages
(around 4 mm deep and 1 mm thick) are placed horizontally above each other,
separated by narrow intervals. The outer surfaces are directed vertically and
the inner surfaces are convex due to the cartilages being thicker in the middle
than at the margins.The first tracheal ring is broader than the rest, and often
divided at one end; it is connected by the cricotracheal ligament with the
lower border of the cricoid cartilage, and is sometimes blended with the next
cartilage down. The last cartilage is thick and broad in the middle, due to its
lower border being prolonged into a triangular hook-shaped (uncinate) process,
which curves downward and backward between the two bronchi. It ends on each
side in an imperfect ring, which encloses the commencement of the bronchus. The
cartilage above the last is somewhat broader than the others at its center.Two
or more of the cartilages often unite, partially or completely, and they are
sometimes bifurcated at their extremities. The rings are generally highly
elastic but they may calcify with age.The trachealis muscle connects the ends
of the incomplete rings and contracts during coughing, reducing the size of the
lumen of the trachea to increase the rate of air flow. The esophagus lies
posteriorly to the trachea, adjoining along the tracheoesophageal stripe.
Circular horizontal bands of fibrous tissue called the annular ligaments of
trachea join the tracheal rings together. The cartilaginous rings are
incomplete to allow the trachea to collapse slightly so that food can pass down
the esophagus. A flap-like epiglottis closes the opening to the larynx during
swallowing to prevent swallowed matter from entering the trachea.
Development
In the fourth week of
embryogenesis as the respiratory bud grows, the trachea separates from the
foregut through the formation of tracheoesophageal ridges which fuse to form
the tracheoesophageal septum and this separates the future trachea from the
oesophagus and divides the foregut tube into the laryngotracheal tube. Before
the end of the fifth week, the trachea begins to develop from the
laryngotracheal tube which develops from the laryngotracheal groove. The first
part of the cephalic region of the tube forms the larynx, and the next part forms
the trachea.
Histology
The trachea is lined with a
layer of pseudostratified columnar epithelium. The epithelium contains goblet
cells, which are glandular, modified simple columnar epithelial cells that
produce mucins, the main component of mucus. Mucus helps to moisten and protect
the airways. Mucus lines the ciliated cells of the trachea to trap inhaled
foreign particles that the cilia then waft upward toward the larynx and then
the pharynx where it can be either swallowed into the stomach or expelled as
phlegm. This self-clearing mechanism is termed mucociliary clearance.
Bronchial Tree
The trachea branches into the
right and left primary bronchi at the carina. These bronchi are also lined by
pseudostratified ciliated columnar epithelium containing mucus-producing goblet
cells. The carina is a raised structure thatcontains specialized nervous tissue
that induces violent coughing if a foreign body, such as food, is present.
Rings ofcartilage, similar to those of the trachea, support the structure of
the bronchi and prevent their collapse. The primary bronchienter the lungs at
the hilum, a concave region where blood vessels, lymphatic vessels, and nerves
also enter the lungs.The bronchi continue to branch into bronchial a tree. A
bronchial tree (or respiratory tree) is the collective term used forthese
multiple-branched bronchi. The main function of the bronchi, like other
conducting zone structures, is to provide apassageway for air to move into and
out of each lung. In addition, the mucous membrane traps debris and pathogens.A
bronchiole branches from the tertiary bronchi. Bronchioles, which are about 1
mm in diameter, further branch until theybecome the tiny terminal bronchioles,
which lead to the structures of gas exchange. There are more than 1000 terminalbronchioles
in each lung. The muscular walls of the bronchioles do not contain cartilage
like those of the bronchi. Thismuscular wall can change the size of the tubing
to increase or decrease airflow through the tube.
Respiratory Zone
In contrast to the conducting
zone, the respiratory zone includes structures that are directly involved in
gas exchange.The respiratory zone begins where the terminal bronchioles join a
respiratory bronchiole, the smallest type of bronchiole, which then leads to an
alveolar duct, opening into a cluster of alveoli. Respiratory Zone Bronchioles
lead to alveolar sacs in the respiratory zone, where gas exchange occurs.
Alveoli
An alveolar duct is a tube composed of smooth
muscle and connective tissue, which opens into a cluster of alveoli. An
alveolus is one of the many small, grape-like sacs that are attached to the
alveolar ducts.An alveolar sac is a cluster of many individual alveoli that are
responsible for gas exchange. An alveolus is approximately 200 mm in diameter
with elastic walls that allow the alveolus to stretch during air intake, which
greatly increases the surface area available for gas exchange. Alveoli are connected
to their neighbors by alveolar pores, which help maintain equal air pressure
throughout the alveoli and lung.

The alveolar wall consists of
three major cell types: type I alveolar cells, type II alveolar cells, and
alveolar macrophages. A type I alveolar cell is a squamous epithelial cell of
the alveoli, which constitute up to 97 percent of the alveolar surface
area.These cells are about 25 nm thick and are highly permeable to gases. A type
II alveolar cell is interspersed among the type I cells and secretes pulmonary
surfactant, a substance composed of phospholipids and proteins that reduces the
surface tension of the alveoli. Roaming around the alveolar wall is the
alveolar macrophage, a phagocytic cell of the immune system that removes debris
and pathogens that have reached the alveoli. The simple squamous epithelium
formed by type I alveolar cells is attached to a thin, elastic basement
membrane. This epithelium is extremely thin and borders the endothelial
membrane of capillaries. Taken together, the alveoli and capillary membranes
form a respiratory membrane that is approximately 0.5 mm thick. The respiratory
membrane allows gases to cross by simple diffusion, allowing oxygen to be picked
up by the blood for transport and CO2 to be released into the air of the
alveoli.
Anatomy of the Lungs
The lungs are pyramid-shaped, paired organs that
are connected to the trachea by the right and left bronchi; on the inferior surface,
the lungs are bordered by the diaphragm. The diaphragm is the flat, dome-shaped
muscle located at the base of the lungs and thoracic cavity. The lungs are
enclosed by the pleurae, which are attached to the mediastinum. The right lung is
shorter and wider than the left lung, and the left lung occupies a smaller
volume than the right. The cardiac notch is an indentation on the surface of
the left lung, and it allows space for the heart . The apex of the lung is the superior
region, whereas the base is the opposite region near the diaphragm. The costal
surface of the lung borders the ribs.The mediastinal surface faces the midline.

Each lung is composed of
smaller units called lobes. Fissures separate these lobes from each other. The
right lung consists of three lobes: the superior, middle, and inferior lobes.
The left lung consists of two lobes: the superior and inferior lobes.A
bronchopulmonary segment is a division of a lobe, and each lobe houses multiple
bronchopulmonary segments. Each segment receives air from its own tertiary
bronchus and is supplied with blood by its own artery. Some diseases of the lungs
typically affect one or more bronchopulmonary segments, and in some cases, the
diseased segments can be surgically removed with little influence on
neighboring segments. A pulmonary lobule is a subdivision formed as the bronchi
branch into bronchioles. Each lobule receives its own large bronchiole that has
multiple branches. An interlobular septum is a wall, composed of connective
tissue, which separates lobules from one another.
Blood Supply and Nervous
Innervation of the Lungs
The blood supply of the lungs
plays an important role in gas exchange and serves as a transport system for
gases throughout the body. In addition, innervation by the both the
parasympathetic and sympathetic nervous systems provides an important level of
control through dilation and constriction of the airway.
Blood Supply
The major function of the
lungs is to perform gas exchange, which requires blood from the pulmonary circulation.
This blood supply contains deoxygenated blood and travels to the lungs where
erythrocytes, also known as red blood cells, pick up oxygen to be transported
to tissues throughout the body. The pulmonary artery is an artery that arises
from the pulmonary trunk and carries deoxygenated, arterial blood to the
alveoli. The pulmonary artery branches multiple times as it follows the
bronchi, and each branch becomes progressively smaller in diameter. One
arteriole and an accompanying venule supply and drain one pulmonary lobule. As
they near the alveoli, the pulmonary arteries become the pulmonary capillary network.
The pulmonary capillary network consists of tiny vessels with very thin walls
that lack smooth muscle fibers. The capillaries branch and follow the
bronchioles and structure of the alveoli. It is at this point that the
capillary wall meets the alveolar wall, creating the respiratory membrane. Once
the blood is oxygenated, it drains from the alveoli by way of multiple
pulmonary veins, which exit the lungs through the hilum.
Nervous Innervation
Dilation and constriction of
the airway are achieved through nervous control by the parasympathetic and
sympathetic nervous systems. The parasympathetic system causes
bronchoconstriction, whereas the sympathetic nervous system stimulates
bronchodilation. Reflexes such as coughing, and the ability of the lungs to
regulate oxygen and carbon dioxide levels, also result from this autonomic
nervous system control. Sensory nerve fibers arise from the vagus nerve, and from
the second to fifth thoracic ganglia. The pulmonary plexus is a region on the
lung root formed by the entrance of the nerves at the hilum. The nerves then
follow the bronchi in the lungs and branch to innervate muscle fibers, glands,
and bloodvessels.
Pleura of the Lungs
Each lung is enclosed within a
cavity that is surrounded by the pleura. The pleura (plural = pleurae) is a
serous membrane that surrounds the lung. The right and left pleurae, which
enclose the right and left lungs, respectively, are separated by the mediastinum.
The pleurae consist of two layers. The visceral pleura is the layer that is
superficial to the lungs, and extends into and lines the lung fissures . In
contrast, the parietal pleura is the outer layer that connects to the thoracic wall,
the mediastinum, and the diaphragm. The visceral and parietal pleurae connect
to each other at the hilum. The pleural cavity is the space between the
visceral and parietal layers.
The pleurae perform two major
functions: They produce pleural fluid and create cavities that separate the
major organs.Pleural fluid is secreted by mesothelial cells from both pleural
layers and acts to lubricate their surfaces. This lubrication reduces friction
between the two layers to prevent trauma during breathing, and creates surface
tension that helps maintain the position of the lungs against the thoracic
wall. This adhesive characteristic of the pleural fluid causes the lungs to
enlarge when the thoracic wall expands during ventilation, allowing the lungs
to fill with air. The pleurae also create a division between major organs that
prevents interference due to the movement of the organs, while preventing the
spread of infection.

Pulmonary ventilation is the act of breathing, which
can be described as the movement of air into and out of the lungs.The major
mechanisms that drive pulmonary ventilation are atmospheric pressure (Patm);
the air pressure within the alveoli,called alveolar pressure (Palv); and the
pressure within the pleural cavity, called intrapleural pressure (Pip).
Mechanisms of Breathing
The alveolar and intrapleural pressures are dependent on
certain physical features of the lung. However, the ability to breathe—to
have air enter the lungs during inspiration and air leave the lungs during
expiration—is dependent on the air pressure of the atmosphere and the
air pressure within the lungs.
Pressure Relationships
Inspiration (or inhalation) and expiration (or exhalation)
are dependent on the differences in pressure between the atmosphere and
the lungs. In a gas, pressure is a force created by the movement of gas molecules
that are confined. For example, a certain number of gas molecules in a
two-liter container has more room than the same number of gas molecules in
a one-liter container. In this case, the force exerted by the movement of the
gas molecules against the walls of the two-liter container is lower than
the force exerted by the gas molecules in the one-liter container. Therefore,
the pressure is lower in the two-liter container and higher in the
one-liter container. At a constant temperature, changing the volume
occupied by the gas changes the pressure, as does changing the number of gas
molecules. Boyle’s law describes the relationship between volume and
pressure in a gas at a constant temperature. Boyle discovered that the pressure
of a gas is inversely proportional to its volume: If volume increases,
pressure decreases. Likewise, if volume decreases, pressure increases.
Pressure and volume are inversely related (P = k/V). Therefore, the pressure in
the one-liter container (one-half the volume of the two-liter container)
would be twice the pressure in the two-liter container. Boyle’s law is
expressed by the following formula:
P1 V1 = P2 V2
In this formula, P1 represents the initial pressure and V1
represents the initial volume, whereas the final pressure and volume are
represented by P2 and V2, respectively. If the two- and one-liter containers
were connected by a tube and the volume of one of the containers were changed,
then the gases would move from higher pressure (lower volume) to lower pressure
(higher volume).

Pulmonary ventilation is dependent on three types of pressure:
atmospheric, intra-alveolar, and interpleural. Atmospheric pressure is the
amount of force that is exerted by gases in the air surrounding any given
surface, such as the body. Atmospheric pressure can be expressed in terms of
the unit atmosphere, abbreviated atm, or in millimeters of mercury (mm Hg). One
atm is equal to 760 mm Hg, which is the atmospheric pressure at sea level.
Typically, for respiration, other pressure values are discussed in relation to
atmospheric pressure. Therefore, negative pressure is pressure lower than the atmospheric
pressure, whereas positive pressure is pressure that it is greater than the
atmospheric pressure. A pressure that is equal to the atmospheric pressure is
expressed as zero. Intra-alveolar pressure is the pressure of the air within
the alveoli, which changes during the different phases of breathing. Because
the alveoli are connected to the atmosphere via the tubing of the airways
(similar to the two- and one-liter containers in the example above), the
interpulmonary pressure of the alveoli always equalizes with the atmospheric pressure.
Intrapleural pressure is the pressure of the air
within the pleural cavity, between the visceral and parietal pleurae. Similar to
intra-alveolar pressure, intrapleural pressure also changes during the
different phases of breathing. However, due to certain characteristics of the
lungs, the intrapleural pressure is always lower than, or negative to, the
intra-alveolar pressure (and therefore also to atmospheric pressure). Although
it fluctuates during inspiration and expiration, intrapleural pressure remains
approximately –4 mm Hg throughout the breathing cycle. Competing forces within
the thorax cause the formation of the negative intrapleural pressure. One of
these forces relates to the elasticity of the lungs themselves—elastic tissue
pulls the lungs inward, away from the thoracic wall. Surface tension of
alveolar fluid, which is mostly water, also creates an inward pull of the lung
tissue. This inward tension from the lungs is countered by opposing forces from
the pleural fluid and thoracic wall. Surface tension within the pleural cavity
pulls the lungs outward. Too much or too little pleural fluid would hinder the
creation of the negative intrapleural pressure; therefore, the level must be
closely monitored by the mesothelial cells and drained by the lymphatic system.
Since the parietal pleura is attached to the thoracic wall, the natural
elasticity of the chest wall opposes the inward pull of the lungs. Ultimately, the
outward pull is slightly greater than the inward pull, creating the –4 mm Hg
intrapleural pressure relative to the intraalveolar pressure. Transpulmonary
pressure is the difference between the intrapleural and intra-alveolar
pressures, and it determines the size of the lungs. A higher transpulmonary
pressure corresponds to a larger lung.
Physical Factors Affecting Ventilation
In addition to the differences in pressures, breathing is
also dependent upon the contraction and relaxation of muscle fibers of both the
diaphragm and thorax. The lungs themselves are passive during breathing,
meaning they are not involved in creating the movement that helps inspiration
and expiration. This is because of the adhesive nature of the pleural fluid, which
allows the lungs to be pulled outward when the thoracic wall moves during
inspiration. The recoil of the thoracic wall during expiration causes
compression of the lungs. Contraction and relaxation of the diaphragm and intercostals
muscles (found between the ribs) cause most of the pressure changes that result
in inspiration and expiration. These muscle movements and subsequent pressure
changes cause air to either rush in or be forced out of the lungs. Other
characteristics of the lungs influence the effort that must be expended to
ventilate. Resistance is a force that slows motion, in this case, the flow of
gases. The size of the airway is the primary factor affecting resistance. A
small tubular diameter forces air through a smaller space, causing more
collisions of air molecules with the walls of the airways. The following
formula helps to describe the relationship between airway resistance and
pressure changes:
F = Δ P / R
As noted earlier, there is
surface tension within the alveoli caused by water present in the lining of the
alveoli. This surface tension tends to inhibit expansion of the alveoli.
However, pulmonary surfactant secreted by type II alveolar cells mixes with
that water and helps reduce this surface tension. Without pulmonary surfactant,
the alveoli would collapse during expiration. Thoracic wall compliance is the
ability of the thoracic wall to stretch while under pressure. This can also
affect the effort expended in the process of breathing. In order for
inspiration to occur, the thoracic cavity must expand. The expansion of the
thoracic cavity directly influences the capacity of the lungs to expand. If the
tissues of the thoracic wall are not very compliant, it will be difficult to
expand the thorax to increase the size of the lungs.
Pulmonary Ventilation
The difference in pressures drives pulmonary ventilation
because air flows down a pressure gradient, that is, air flows from an area of
higher pressure to an area of lower pressure. Air flows into the lungs largely
due to a difference in pressure; atmospheric pressure is greater than
intra-alveolar pressure, and intra-alveolar pressure is greater than
intrapleural pressure. Air flows out of the lungs during expiration based on
the same principle; pressure within the lungs becomes greater than the atmospheric
pressure. Pulmonary ventilation comprises two major steps: inspiration and
expiration. Inspiration is the process that causes air to enter the lungs, and
expiration is the process that causes air to leave the lungs . A respiratory
cycle is one sequence of inspiration and expiration. In general, two muscle
groups are used during normal inspiration: the diaphragm and the external
intercostal muscles. Additional muscles can be used if a bigger breath is
required. When the diaphragm contracts, it moves inferiorly toward the
abdominal cavity, creating a larger thoracic cavity and more space for the
lungs. Contraction of the external intercostal muscles moves the ribs upward
and outward, causing the rib cage to expand, which increases the volume of the
thoracic cavity. Due to the adhesive force of the pleural fluid, the expansion
of the thoracic cavity forces the lungs to stretch and expand as well. This
increase in volume leads to a decrease in intra-alveolar pressure, creating a
pressure lower than atmospheric pressure. As a result, a pressure gradient is
created that drives air into the lungs.
The process of normal expiration is passive, meaning that
energy is not required to push air out of the lungs. Instead, the elasticity of
the lung tissue causes the lung to recoil, as the diaphragm and intercostal
muscles relax following inspiration. In turn, the thoracic cavity and lungs
decrease in volume, causing an increase in interpulmonary pressure. The
interpulmonary pressure rises above atmospheric pressure, creating a pressure
gradient that causes air to leave the lungs. There are different types, or
modes, of breathing that require a slightly different process to allow
inspiration and expiration. Quiet breathing, also known as eupnea, is a mode of
breathing that occurs at rest and does not require the cognitive thought of the
individual. During quiet breathing, the diaphragm and external intercostals
must contract.
A deep breath, called diaphragmatic breathing, requires the
diaphragm to contract. As the diaphragm relaxes, air passively leaves the
lungs. A shallow breath, called costal breathing, requires contraction of the
intercostal muscles. As the intercostals muscles relax, air passively leaves
the lungs. In contrast, forced breathing, also known as hyperpnea, is a mode of
breathing that can occur during exercise or actions that require the active
manipulation of breathing, such as singing. During forced breathing,
inspiration and expiration both occur due to muscle contractions. In addition to
the contraction of the diaphragm and intercostal muscles, other accessory muscles
must also contract. During forced inspiration, muscles of the neck, including
the scalenes, contract and lift the thoracic wall, increasing lung volume.
During forced expiration, accessory muscles of the abdomen, including the
obliques, contract, forcing abdominal organs upward against the diaphragm. This
helps to push the diaphragm further into the thorax, pushing more air out. In
addition, accessory muscles (primarily the internal intercostals) help to
compress the rib cage, which also reduces the volume of the thoracic cavity.
Respiratory Volumes and Capacities
Respiratory volume is the term used for various volumes of
air moved by or associated with the lungs at a given point in the respiratory
cycle. There are four major types of respiratory volumes: tidal, residual,
inspiratory reserve, and expiratory reserve . Tidal volume (TV) is the amount
of air that normally enters the lungs during quiet breathing, which is about
500 milliliters. Expiratory reserve volume (ERV) is the amount of air you can
forcefully exhale past a normal tidal expiration, up to 1200 milliliters for
men. Inspiratory reserve volume (IRV) is produced by a deep inhalation, past a
tidal inspiration. This is the extra volume that can be brought into the lungs
during a forced inspiration. Residual volume (RV) is the air left in the lungs
if you exhale as much air as possible. The residual volume makes breathing
easier by preventing the alveoli from collapsing. Respiratory volume is
dependent on a variety of factors, and measuring the different types of respiratory
volumes can provide important clues about a person’s respiratory health.
Respiratory capacity is the combination of two or more
selected volumes, which further describes the amount of air in the lungs during
a given time. For example, total lung capacity (TLC) is the sum of all of the
lung volumes (TV, ERV, IRV, and RV), which represents the total amount of air a
person can hold in the lungs after a forceful inhalation. TLC is about 6000 mL
air for men, and about 4200 mL for women. Vital capacity (VC) is the amount of
air a person can move into or out of his or her lungs, and is the sum of all of
the volumes except residual volume (TV, ERV, and IRV), which is between 4000
and 5000 milliliters. Inspiratory capacity (IC) is the maximum amount of air
that can be inhaled past a normal tidal expiration, is the sum of the tidal
volume and inspiratory reserve volume. On the other hand, the functional
residual capacity (FRC) is the amount of air that remains in the lung after a
normal tidal expiration; it is the sum of expiratory reserve volume and residual
volume.
In addition to the air that creates respiratory volumes, the
respiratory system also contains anatomical dead space, which is air that is
present in the airway that never reaches the alveoli and therefore never
participates in gas exchange. Alveolar dead space involves air found within
alveoli that are unable to function, such as those affected by disease or
abnormal blood flow. Total dead space is the anatomical dead space and alveolar
dead space together, and represents all of the air in the respiratory system
that is not being used in the gas exchange process.
Respiratory Rate and Control of Ventilation
Breathing usually occurs without thought, although at times
you can consciously control it, such as when you swim under water, sing a song,
or blow bubbles. The respiratory rate is the total number of breaths, or
respiratory cycles, that occur each minute. Respiratory rate can be an
important indicator of disease, as the rate may increase or decrease during an
illness or in a disease condition. The respiratory rate is controlled by the
respiratory center located within the medulla oblongata in the brain, which
responds primarily to changes in carbon dioxide, oxygen, and pH levels in the
blood. The normal respiratory rate of a child decreases from birth to
adolescence. A child under 1 year of age has a normal respiratory rate between
30 and 60 breaths per minute, but by the time a child is about 10 years old,
the normal rate is closer to 18 to 30. By adolescence, the normal respiratory
rate is similar to that of adults, 12 to 18 breaths per minute.
Ventilation Control Centers
The control of ventilation is a complex interplay of
multiple regions in the brain that signal the muscles used in pulmonary ventilation
to contract . The result is typically a rhythmic, consistent ventilation rate
that provides the body with sufficient amounts of oxygen, while adequately
removing carbon dioxide.The medulla oblongata contains the dorsal respiratory
group (DRG) and the ventral respiratory group (VRG). The DRG is involved in
maintaining a constant breathing rhythm by stimulating the diaphragm and
intercostal muscles to contract, resulting in inspiration. When activity in the
DRG ceases, it no longer stimulates the diaphragm and intercostals to contract,
allowing them to relax, resulting in expiration. The VRG is involved in forced
breathing, as the neurons in the VRG stimulate the accessory muscles involved
in forced breathing to contract, resulting in forced inspiration. The VRG also
stimulates the accessory muscles involved in forced expiration to contract. The
second respiratory center of the brain is located within the pons, called the
pontine respiratory group, and consists of the apneustic and pneumotaxic
centers. The apneustic center is a double cluster of neuronal cell bodies that
stimulate neurons in the DRG, controlling the depth of inspiration,
particularly for deep breathing. The pneumotaxic center is a network of neurons
that inhibits the activity of neurons in the DRG, allowing relaxation after
inspiration, and thus controlling the overall rate. Factors That Affect the
Rate and Depth of Respiration The respiratory rate and the depth of inspiration
are regulated by the medulla oblongata and pons; however, these regions of the
brain do so in response to systemic stimuli. It is a dose-response,
positive-feedback relationship in which the greater the stimulus, the greater
the response. Thus, increasing stimuli results in forced breathing. Multiple
systemic factors are involved in stimulating the brain to produce pulmonary
ventilation. The major factor that stimulates the medulla oblongata and pons to
produce respiration is surprisingly not oxygen concentration, but rather the
concentration of carbon dioxide in the blood. As you recall, carbon dioxide is
a waste product of cellular respiration and can be toxic. Concentrations of
chemicals are sensed by chemoreceptors. A central chemoreceptor is one of the
specialized receptors that are located in the brain and brainstem, whereas a
peripheral chemoreceptor is one of the specialized receptors located in the
carotid arteries and aortic arch. Concentration changes in certain substances,
such as carbon dioxide or hydrogen ions, stimulate these receptors, which in
turn signal the respiration centers of the brain. In the case of carbon
dioxide, as the concentration of CO2 in the blood increases, it readily
diffuses across the blood-brain barrier, where it collects in the extracellular
fluid. As will be explained in more detail later, increased carbon dioxide
levels lead to increased levels of hydrogen ions, decreasing pH. The increase
in hydrogen ions in the brain triggers the central chemoreceptors to stimulate
the respiratory centers to initiate contraction of the diaphragm and intercostal
muscles. As a result, the rate and depth of respiration increase, allowing more
carbon dioxide to be expelled, which brings more air into and out of the lungs
promoting a reduction in the blood levels of carbon dioxide, and therefore hydrogen
ions, in the blood. In contrast, low levels of carbon dioxide in the blood
cause low levels of hydrogen ions in the brain, leading to a decrease in the
rate and depth of pulmonary ventilation, producing shallow, slow breathing. Another
factor involved in influencing the respiratory activity of the brain is
systemic arterial concentrations of hydrogen ions. Increasing carbon dioxide
levels can lead to increased H+ levels, as mentioned above, as well as other
metabolic activities, such as lactic acid accumulation after strenuous
exercise. Peripheral chemoreceptors of the aortic arch and carotid arteries
sense arterial levels of hydrogen ions. When peripheral chemoreceptors sense
decreasing, or more acidic, pH levels, they stimulate an increase in ventilation
to remove carbon dioxide from the blood at a quicker rate. Removal of carbon dioxide
from the blood helps to reduce hydrogen ions, thus increasing systemic pH.Blood
levels of oxygen are also important in influencing respiratory rate. The
peripheral chemoreceptors are responsible for sensing large changes in blood
oxygen levels. If blood oxygen levels become quite low—about 60 mm Hg or
less—then peripheral chemoreceptors stimulate an increase in respiratory
activity. The chemoreceptors are only able to sense dissolved oxygen molecules,
not the oxygen that is bound to hemoglobin. As you recall, the majority of
oxygen is bound by hemoglobin; when dissolved levels of oxygen drop, hemoglobin
releases oxygen. Therefore, a large drop in oxygen levels is required to
stimulate the chemoreceptors of the aortic arch and carotid arteries. The
hypothalamus and other brain regions associated with the limbic system also
play roles in influencing the regulation of breathing by interacting with the
respiratory centers. The hypothalamus and other regions associated with the
limbic system are involved in regulating respiration in response to emotions,
pain, and temperature. For example, an increase in body temperature causes an
increase in respiratory rate. Feeling excited or the fight-or-flight response
will also result in an increase in respiratory rate.
Transporting the Gases
The gas exchange process
necessary for cells to function properly could not occur without the blood
transporting oxygen and carbon dioxide throughout the body. This transportation
depends on the gases’ distinct properties and on a blood component called
hemoglobin, an oxygen carrying protein found in red blood cells called erythrocytes.
O2 Transport
Compared to carbon dioxide,
oxygen is not very soluble. As a result, only about 0.01 fluid ounces (0.3
milliliters) of oxygen will dissolve in every 3.4 fluid ounces (100
milliliters) of blood plasma, which is not enough to carry sufficient oxygen to
the body’s tissues and cells. The majority of oxygen in the human body is
carried via hemoglobin, which is the respiratory pigment in humans and also
gives blood its red color. Because of the affinity of oxygen to hemoglobin, the
oxygen-carrying capacity of blood is boosted nearly 70-fold to about 0.7 fluid
ounces (20.8 milliliters) per 3.4 fluid ounces (100 milliliters) of blood. Hemoglobin’s
unique molecular characteristics make it an excellent transport molecule for
oxygen. Each hemoglobin molecule includes four hemes, which are iron-containing
porphyrin compounds, combined with the protein globin. Porphyrins are a group
of organic pigments characterized by a ringed group of four linked
nitrogen-containing molecular rings (called a tetrapyrrole nucleus). In a heme,
each porphyrin ring has an atom of iron (Fe) at its center. Each iron atom can
unite with one molecule of oxygen. As a result, each hemoglobin molecule can
carry four oxygen molecules. Furthermore, when one oxygen molecule binds to one
of the four heme groups, the other heme groups change shape ever so slightly so
that their affinity increases for the binding of each subsequent oxygen molecule.
In other words, after the first oxygen molecule is attached, the next three
oxygen molecules attach even more rapidly to form oxyhemoglobin (the bright red
hemoglobin that is a combination of hemoglobin and oxygen from the lungs), thus
providing rapid transfer of oxygen throughout the blood. Conversely, when it
comes time for hemoglobin to “unload” its oxygen content into cells and
tissues, once one heme group releases its oxygen, the other three rapidly
follow.
Oxygen’s affinity for hemoglobin
is also affected by the partial pressure of carbon dioxide and the blood’s pH
level. This is known as the Bohr effect, named after its discoverer Christian
Bohr (1855–1911). A high concentration, or partial pressure, of carbon dioxide
makes the blood more acidic, which causes hemoglobin to have less affinity for
oxygen. As a result, in tissues in which the concentration of carbon dioxide in
the blood is high because of its release as a waste product from cells,
hemoglobin easily releases oxygen. In the lungs, where blood carbon dioxide levels
are low because of its diffusion into the alveoli, hemoglobin readily accepts
oxygen. The Bohr effect or shift, which relates to a mathematically plotted
curve called the oxygen dissociation curve, serves an extremely useful purpose.
During exercise, cells are working harder—more actively respiring—to produce
more energy. As a result, they release much higher levels of carbon dioxide
into the blood than when the body is at rest. The higher carbon dioxide levels,
in turn, reduce the blood’s pH level, thus acidifying the blood and signaling
hemoglobin to release more rapidly the oxygen needed to replenish cells and
tissues. In other words, the Bohr effect informs the body that its metabolism
has increased due to exercise and that it must compensate for the increased
need to absorb oxygen and release carbon dioxide.
CO2 Transport
Carbon dioxide enters the blood
as a waste product of cell metabolism and cellular respiration. Unlike oxygen,
carbon dioxide readily dissolves in blood. Carbon dioxide is transported by the
blood to the alveoli in three ways:
1. As soluble CO2 in blood (5–10
percent)
2. Bound by hemoglobin (20–30
percent)
3. As a bicarbonate (60–70
percent)
Although carbon dioxide is more
soluble than oxygen and dissolves directly into the blood after it diffuses out
of cells, the amount that dissolves is not enough to perform the essential
function of ridding the body of carbon dioxide. In the second mode of
transport, approximately a quarter of the carbon dioxide eliminated from cells
reacts with hemoglobin.
In essence, carbon dioxide is
able to hitch a ride with hemoglobin because, at this point, hemoglobin is not
carrying much oxygen and has an increased affinity for carbon dioxide. This is
known as the Haldane effect and occurs as blood passes through the lungs. Blood
proteins that bind to carbon dioxide are called carbamino compounds. When
carbon dioxide binds to the hemoglobin’s protein, the combination is called
carbaminohemoglobin. The first two methods of transporting carbon dioxide are
relatively slow and inefficient compared to the third method of transporting
the gas. Because carbon dioxide is highly soluble, it reacts readily with water
(H2O) molecules to form carbonic acid (H2CO3) in red blood cells. This reaction
would also be too slow for efficient carbon dioxide transport if not for an
enzyme called carbonic anhydrase (CA), which is highly concentrated in red
blood cells and acts as a catalyst to help produce carbonic acid. The carbonic
acid then ionizes (or disassociates) to form a positively charged hydrogen ion
(H+) and a negatively charged bicarbonate ion (HCO3−). The chemical process can
be viewed as follows:
CO2 + H2O !! H2CO3 !! H+ + HCO3
Because the concentration of the
negatively charged bicarbonate ions in the red blood cells is at a higher level
than outside of these cells, these ions readily diffuse into the surrounding
blood plasma for transport to the alveoli. To compensate for the negatively
charged bicarbonate ions moving out of a red blood cell, a negatively charge
chloride (Cl) ion enters the cell from the plasma to maintain the electrical
balance in both the erythrocyte and the plasma. This exchange is called a
chloride shift.
Cellular Respiration
Cellular respiration is the
process by which cells use the oxygen delivered by the respiratory and
circulatory systems to manufacture and release the chemical energy stored in
food, primarily in the form of carbohydrates. As such, it is called an
exergonic reaction, meaning that it produces energy. Cellular respiration
produces energy via a catabolic process, that is, by making smaller things out
of larger things. In cellular respiration, it refers to the breaking down of
polymers (large molecules formed by the chemical linking of many smaller
molecules) into smaller and more manageable molecules. The catabolic process
within cells involves breaking down glucose, a simple sugar in carbohydrates
that stores energy, into smaller molecules called pyruvic acid. These
smallermolecules are ultimately used to produce adenosine triphosphate (ATP).
ATP is the primary “energy currency” of the cell, the human body, and nearly
all forms of life. Energy via ATP in cells is used to:
• Manufacture proteins
• Construct new organelles
(subcellular structures that perform a role within each cell)
• Replicate DNA
• Synthesize fats and
polysaccharides
• Pump water through cell
membranes
• Contract muscles
• Conduct nerve impulses
Cellular respiration is the most
efficient catabolic process known to exist in nature. Although it occurs in
every cell in the body, cellular respiration does not take place simultaneously
in the exact same phases throughout all the cells. If the energy produced though
cellular respiration was released simultaneously, the body would not be able to
process all the energy efficiently, which would result in wasted energy. In
addition, the impact of such a large amount of energy being released all at
once could overload and damage cells. As a result, cellular respiration occurs
at different stages in the body’s various cells, even in cells that are close
neighbors or side by side. ATP molecules act like time-release capsules; they release
small amounts of energy to fuel various functions within the body at different
times. Overall, two primary processes occur in cellular respiration. The first is
the breakdown of glucose into carbon dioxide and hydrogen, known as the carbon
pathway. The second is the transfer of hydrogen from sugar molecules to oxygen,
resulting in the creation of water and energy. The entire process of cellular
respiration occurs in three primary stages:
1. Glycolysis
2. Krebs cycle (citric acid cycle)
3. Electron transport system
Glycolysis
Glycolysis, which comes from the
Greek words glykos (“sugar” or “sweet”) and lysis (“splitting”), is the initial
harvester of chemical energy within the body. It occurs in the cell’s cytoplasm
and converts glucose molecules into molecules of pyruvate, or pyruvic acid.
Unlike the other processes in cellular respiration, glycolysis does not require
oxygen and is the only metabolic pathway shared by all living organisms.
Scientists believe that this biological approach to producing life-giving
energy existed before oxygen developed in the Earth’s atmosphere. It is the
first step in both aerobic (oxygen) and anaerobic (oxygen-free) energyproducing
processes .Glycolysis is a multistep process, with each step being catalyzed by
a specific enzyme dissolved in the fluid portion of the cytoplasm called the cytosol.
As with all biological processes, energy is needed to begin the process, and
two ATP energy molecules initiate the reactions. This initial input of energy
is called the energy investment phase, and occurs when ATP is used to
phosphorylate, or add a phosphate to, the six-carbon glucose molecule. However,
the process also yields energy in that further breaking down the six-carbon
glucose molecule into two three-carbon pyruvic acid molecules ultimately
results in a net gain of ATP molecules, as well as other energy molecules such
as reduced nicotinamide adenine dinucleotide (NADH). However, glycolysis is
extremely inefficient. The entire process captures only about 2 percent of the
energy that is available in glucose for use by the body. Much more energy is
available in the two molecules of pyruvic acid and NADH produced during
glycolysis. It is this potential energy that goes on to the next step, called
the Krebs cycle.
Anaerobic Respiration
When we exercise, our bodies
produce more energy and require more oxygen. However, our blood cannot always supply
enough of the oxygen via respiration that the cells in our muscles need. Under
these circumstances, our muscle cells can respire anaerobically, that is,
without oxygen, like some fungi and bacteria are able to do. Anaerobic
respiration is also referred to as fermentation. However, cells in the human
body can only respire without oxygen for a short period of time. Like normal
aerobic cellular respiration, anaerobic respiration begins with glucose in the
cell, but takes place completely in the cell’s cytoplasm. Although ATP energy
molecules are also produced this way, the process is extremely inefficient
compared to aerobic respiration. In the human body, the anaerobic process
results in pyruvic acid being turned into the waste product lactic acid, as
opposed to entering the mitochondria for further oxidation as it does in
aerobic cellular respiration. It is the lactic acid in muscles that makes them
stiff and sore after intense aerobic exercise, such as running.
The Krebs Cycle (Citric Acid
Cycle)
Discovered by Hans Krebs
(1900–1981), the Krebs cycle, also known as the citric acid cycle, is a cyclic
series of molecular reactions that require oxygen to function. The cycle is
mediated by enzymes that help create the molecules for the final harvesting of
cellular energy in the third and final phase of the cellular respiration
process. The Krebs cycle occurs in the matrix of the mitochondria, which are
the powerhouses of cells. Although the mitochondrion is the second largest
organelle in a cell after the nucleus, some cells may contain thousands of
mitochondria from 0.5 to 1 micrometer in diameter. Unlike the energy-harvesting
process of glycolysis in the cytoplasm, mitochondria are extremely efficient in
taking energy from sugar (and other nutrients) and converting it into ATP. In
fact, compared to the typical automobile engine, which only harvests about 25
percent of the energy available in gasoline to propel a car, the mitochondrion is
more than twice as efficient—it converts 54 percent of the energy available in
sugar into ATP. After glycolysis is completed, the two pyruvate molecules that
were formed enter the mitochondria for complete oxidization by a series of reactions
mediated by various enzymes. As the pyruvate leaves the cytoplasm and enters a
mitochondrion, acetyl coenzyme A (CoA) is produced when an enzyme removes
carbon and oxygen molecules from each pyruvate molecule. This step is known as
the transition reaction. The Krebs cycle begins as oxygen within the cells is
used to completely oxidize the acetyl CoA molecules. The process is initiated
when each of the acetyl CoA molecules combines with oxaloacetic acid to produce
a six-carbon citric acid molecule. Further oxidation eventually produces a
four-carbon compound and carbon dioxide. The four-carbon compound is ultimately
transformed back in oxaloacetic acid so that the cycle can begin again. Because
two pyruvate molecules are transferred into the mitochondria for each glucose
molecule, the cycle must be completed twice, once for each pyruvate molecule.
Each cycle results in one molecule of ATP, two molecules of carbon dioxide, and
eight hydrogen molecules. The ATP molecules produced during this cycle can be
used as energy. But it is through the cycle’s creation of the electron
“carrier” coenzyme molecules NADH and reduced flavin adenine dinucleotide (FADH2)—which
are created when the coenzymes nicotine adenine dinucleotide (NAD) and flavin
adenine dinucleotide (FAD) “pick up” the hydrogen molecules—that the abundance
of ATP is produced in the next stage of cellular respiration, the electron
transport system.
Electron Transport System
Overall, the first two processes
in cellular respiration, glycolysis and the Krebs cycle, have produced
relatively little energy for the body’s cells to use. Although both of these
processes produce some ATP directly, the energy currency of ATP is created and
cashed in for the big payoff during the electron transport system, also known as
the electron transport chain. This process takes place across the inner
membrane of the mitochondria called the cristae. A chain of electron receptors
are embedded in the cristae, which are folded to create numerous inward,
parallel, regularly spaced projections or ridges. This design results in an
extremely high density of receptors, thus increasing the electron transport
chain’s efficiency. The receptors are actually a network of proteins that can
carry electrons and transfer them on down a protein chain. The process works
like a snowball gaining speed as it rolls down a hill. As the NADH and FADH2 molecules
produced during glycolysis and the Krebs cycle pass down the chain, they
release electrons to the first molecule in the chain and so on. Because each
successive carrier in the chain is higher in electronegativity (that is, has a
higher tendency to attract electrons) than the previous carrier, the electrons
are “pulled downhill.” During the process, hydrogen protons (H+) or ions from
NADH and FADH2 are transferred along a group of closely related protein
receptors that include flavoproteins, iron-sulfur proteins, quinones, and a
group of proteins called cytochromes. The cytochrome proteins in the electron
transport system will only accept the electron from each hydrogen and not the
entire atom. The final cytochrome carrier in the chain transfers the electrons,
which by this time have lost all their energy, to oxygen in the matrix to
create the hydrogen-oxygen bond of water. This bond is another reason why
oxygen is so important to the life of the cell. Without it, the molecules in
the chain would remain stuck with electrons, and ATP would not be produced. Because
of the second law of thermodynamics, the electrons passed down the chain lose
some of their energy with every transfer from cytochrome to cytochrome. Some of
the energy lost helps to “pump” hydrogen ions out of the mitochondria’s matrix
into a confined intermembrane space between the mitochondria’s inner and outer
membranes. This energy for pumping the hydrogen ions is a result of a process
called the oxidationreduction reaction, or redox reaction. The reaction results
in the molecules within the electron transport system alternately being reduced
(gaining an electron) and then oxidized (losing an electron). The entire
process establishes a buildup of hydrogen ions, resulting in a concentration,
or diffusion, gradient—more hydrogen ions are pumped inside the confined space
between the mitochondria’s membranes than exist in the mitochondria’s matrix.
As the concentration gradient increases, the ions begin to diffuse back through
the membrane into the matrix to equalize the hydrogen ion gradient. Hydrogen
ion diffusion occurs through ATP synthase, an enzyme within the inner membrane
of the mitochondrion. ATP synthase uses the potential energy of the proton
gradient to synthesize the abundance of ATP out of the adenosine diphosphate
(ADP) molecule and phosphate. This process is referred to as chemiosmosis. The
formation of ATP is an energy storage process, and the energy is released when
ATP is converted via the ATPase enzyme back into ADP (adenose bound to two
phosphate groups) or to adenosine monophosphate (AMP—adenose bound to one phosphate
group). All of these conversions are known as ATP phosphorylation. ADP and the
separate phosphates produced by the breakdown are then recycled into cellular
respiration for the recreation of ATP. At the same time, the waste products
carbon dioxide and water are eliminated via diffusion from the cell into the
bloodstream and on through the organismal respiratory process .
Synthesis of ATP.
The buildup of hydrogen ions into
the mitochondria’s intermembrane space via electron transport and the eventual
transport of these ions back through the membrane, where they are used by ATP
synthase to make ATP (the major source of energy for cellular reactions) out of
ADP and phosphate. (Sandy Windelspecht/ Ricochet Productions)
Respiratory System Defense
Mechanisms
The respiratory systemhas several
features that help protect it from the possible harmful effects of
environmental particles and pathogens (viruses, bacteria, etc.) that can enter
the system when we breathe. In the upper respiratory tract, the mucociliary
(mucus and ciliary) lining of the nasal cavity is the respiratory system’s first
line of defense. Composed of tiny hairs lining the nose, this defense mechanism
filters out the particles inhaled from the environment. The second line of
defense is the mucus that lines the turbinate bones (scrolled spongy bones of
the nasal passages) in the sinuses and collects particles that get past the
nose. These defense mechanisms together trap larger particles from 5 to 10
micrometers in diameter.
As the air we breathe passes
through the nose and nasal cavity, it enters the pharynx, where many particles
also stick to the mucus on the back of the throat and tonsils. These captured
particles can then be eliminated via coughing and sneezing. In addition, the
adenoids and tonsils in the back of the throat help trap pathogens for
elimination. These lymphoid tissues (tissue from the lymphatic system) also play
an important role in developing an immune system response, such as the
production of antibodies to fight off germs. The lower portion of the
respiratory tract also has ciliated cells and mucus-secreting cells that cover
it with a layer of mucus. These features work together with the mucus-trapping
particles and pathogens, which are then driven upwards by the sweeping ciliary
action to the back of the throat where they can be expelled. Most of the upper
respiratory tract surfaces (including the nasal and oral passages, the pharynx,
and the trachea) are colonized by a variety of naturally occurring organisms
called flora. These organisms (primarily of the staphylococcus group) can help
to combat infections and maintain a healthy respiratory system by preventing
infectious microorganisms or pathogens from getting a foothold. This phenomenon
is known as colonization resistance or inhibition, and occurs because the
normal flora compete for space and nutrients in the body. Some flora also
produce toxins that are harmful to other pathogenic microorganisms. In rare
instances, normal flora can help cause disease if outside factors cause them to
become pathogenic or they are introduced into normally sterile sites in the
body.Despite these defense mechanisms, pathogens and particles from 2 to 0.2micrometers
oftenmake their way to the lungs and the alveoli. For example, most bacteria
and all viruses are 2 micrometers or smaller. The alveoli, however, also have
defense mechanisms to protect against microscopic invaders. In the case of the
lungs, these mechanisms are primarily cellular in nature. For example, alveolar
macrophages are a type of leukocyte that ingest and destroy invading organisms
as part of the immune system’s response to infection. The fluid lining the
alveoli contains many components, such as surfactant, phospholipids, and other
unidentified agents, thatmay be important in activating alveolar macrophages.
Lymphoid tissue associated with the lungs also plays a role in defending
against infections by initiating immune responses. For example, immune system cells,
such as B and T cells, represent a local immune response to fight off infections
by producing antibodies or activating macrophages.